Content warning: This story contains language that pertains to mental health and suicide.
I couldn’t breathe. My lungs spasmed, desperate for air as my eyes darted across the room. The knot in my stomach twisted, tightening with each tick of the clock.
My mind, corrupted with a million thoughts, redirected its focus to a sole question: Is this what it feels like to go insane?
It was early June of 2023 and I had just started taking Lexapro, an antidepressant commonly prescribed to people who struggle with anxiety or depression.
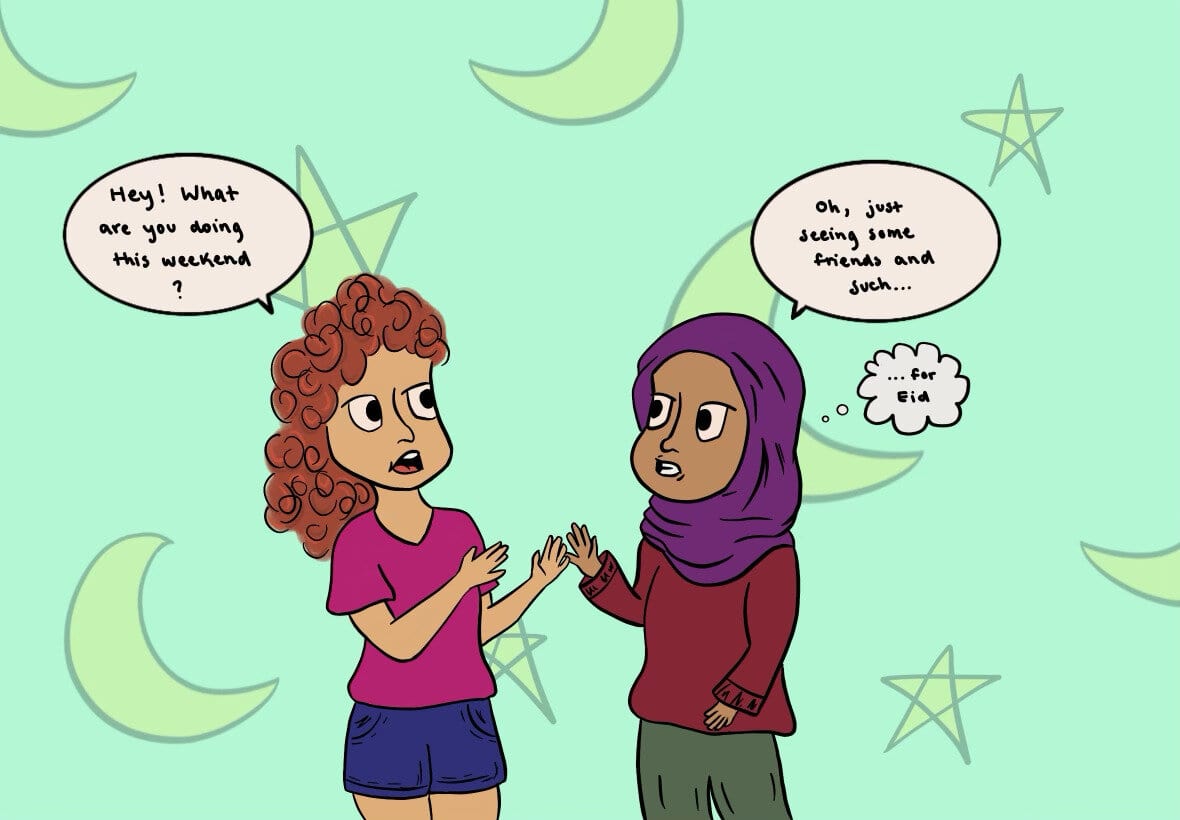
The fact that I was even taking medication was a surprise to everyone around me. I had been struggling with debilitating anxiety for almost my entire life, but I had become incredibly adept at hiding my distress. It took a near breakdown before my parents took notice and convinced me to get help. By the time I finally showed up at my doctor’s office, I was desperate for any relief from the racing worries that consumed me.
My doctor and I decided that the best course of action was to start antidepressants in conjunction with therapy. The doctor mentioned that there could be side effects from the medication, but I thought that was an obligated statement rather than an actual warning.
I wasn’t prepared for it to leave me curled up on a ball on the edge of my bedsheets, shaking uncontrollably. I wasn’t prepared to get on the bus in the morning, unable to move due to the feeling of dread that embedded itself into my limbs.
Sleepless nights turned into sleepless weeks, which turned into nearly a month of deep depression. Despite my anguish, I maintained a persona: I was still a high-achieving student with a seemingly perfect life. But it only took the shutting of my bedroom door for the mask to slip away and leave me alone with my pain.
In these moments, I felt like there was nothing I could do to escape, but the ironic truth is that there was a very easy escape: I could stop taking the medicine and contact my doctor. Yet, every night, I gulped down the capsule.
I was wholly convinced that if I waited just a little while longer, the medication would kick in and start producing the desired effect. I was sure that if I gave up on this drug, I would never rid myself of the mental illness that drove me to it in the first place. These worries are all too common among struggling adolescents, who often believe that if one solution doesn’t work, their situation is hopeless.
In this moment of extreme desperation, the obvious solution, seeing a doctor, never crossed my mind. I wrote, “I’m just always going to be in pain. I can’t take it. I can’t do this. I’m so sorry.”
After a month of routine distress, I hit my breaking point. I had to quit my job the next day, and I was petrified. I was awake for hours, spiraling between extreme fear and a desperation to escape it, having constant panic attacks. I felt like I was in danger of hurting myself.
That night at nearly two in the morning, I went downstairs to find my dad. Through stifled tears I told him that I needed to go back to the doctor. He agreed, his face painted with deep-seated fear. He made me promise to stop the medicine immediately and made an appointment for the following week.
After I stopped the medication, I almost immediately noticed changes in my mental state. Even though I was experiencing the same anxiety that had pushed me to start medication, at this point it was a relief. After my experience on Lexapro, any relief was enough.
In the days between stopping my medication and the doctor’s appointment, I considered my next steps. My doctor couldn’t tell me what to do, she could only advise based on the experience I had explained.
Before even entering the doctor’s office I had decided that I wanted to try another medication. I wasn’t going to give up on long-term relief just because I had hit a painful roadblock. My doctor agreed with my decision, and suggested I start Zoloft, a different medication in the same drug class.
The night I was supposed to start taking Zoloft, I stared at my translucent pill box, terrified to swallow the capsule. What if it didn’t work? What if it left me in the same position as before? The previous drug left me mentally paralyzed, so why was I somehow willing to put myself in that danger again?
Despite my fear, I forced myself to swallow the pill. I had survived the pain once, and I knew I could do it again. The faint possibility of true relief outweighed the looming danger of more side effects. The medication would either work or it wouldn’t, but I was prepared for each possibility.
15 weeks after taking the new medication, I can confidently say that forcing myself to swallow that pill was the right decision. More than anything else, the medication has made me happier — my worries don’t consume me so absolutely, and I’m able to more easily let go of my negative thoughts.
There’s no question that I still have stressful moments. I still worry about tests, and I still scroll anxiously through Instagram. The crucial word though is moments — I have my moments, but I don’t have a life full of them.
I can breathe again.
When I was in the midst of taking the first medicine, I thought there was no hope for me if it didn’t work. I was totally convinced that I had used up all of my options, but my experience opened me to the falsehood in this perception — there are so many interventional options for people who are struggling. There are different classes of medicine, different therapeutic approaches and even new experimental treatments.
As someone who’s been through it, I can confidently say that things can and will get better. It is worth taking the winding path to recovery, even if it seems impossible and never-ending. The excruciating journey will end, and when it does you’ll be happy you chose not to give up.
If you or someone you know is experiencing suicidal thoughts or ideation, please call or text 988.